Incontinence means poor control of the bladder and bowel. It affects many people after a stroke. Sometimes incontinence is caused by your brain having trouble communicating with your body. Also, you may have difficulties getting to the bathroom or taking clothes off in time. If you already had bowel or bladder problems before the stroke, the incontinence may have become worse.
Sometimes medication can affect your bladder and bowel. If that is the case for you, speak with your doctor about it. Do not stop any medication without first speaking with your doctor.
Many people recover control of their bladder and bowel function soon after stroke. For other people, some problems may continue for a longer time.
Bladder problems
There are several types of bladder problem:
- Urinary incontinence is the loss of control of your bladder.
- Urinary frequency is the need to use the toilet more often.
- Urge incontinence is the sudden need or urge to urinate.
- Functional incontinence means trouble getting to the toilet in time or trouble getting clothes off soon enough.
- Night time (nocturnal) incontinence is the need to use the toilet several times during the night, or urinating the bed at night.
- Stress incontinence is loss of bladder control due to pressure on the abdomen. For example, urinating after sneezing or exercise.
Urinary tract infection
Problems with emptying the bladder can lead to urinary tract infection. Contact your doctor if you see signs of infection. Symptoms include:
- feeling the need to urinate, even if the bladder is empty
- losing control of your bladder (urinary incontinence)
- pain or burning while urinating
- stomach cramps
- cloudy urine or urine with a strong smell
- fever or increased body temperature
- a sudden change in behaviour.

Chuck & Lorraine share an unshakable bond after facing stroke together.

Bowel problems
Bowel problems can occur after a stroke:
- Constipation develops when bowel movements do not occur as often as they used to or you have trouble passing stools.
- Diarrhea is loose bowel movements.
- Bowel incontinence is the loss of control of the muscles around your lower bowel.
- Functional bowel incontinence means trouble getting to the toilet in time or trouble getting clothes off soon enough.
Strategies for dealing with bladder and bowel problems
Talk to your healthcare team about what is causing your problem. They can help you understand the cause and suggest strategies to deal with it. Here are some common strategies:

Make getting to the bathroom easier.
- Clear a path. Remove any items, such as furniture or mats that block your way to the toilet.
- Install a night light.
- Use a raised toilet seat. These come with or without armrests and make it easier and safer to get on and off.
- If getting on or off the toilet is too hard or unsafe, use a commode (portable toilet) or urinal. This can be particularly helpful at night.
When control is lost
If you are unable to control your bladder, continence products will help keep you dry. Be sure to use continence products, not menstrual pads. Continence products are better at drawing the urine away to promote healthier skin.
Constipation
To help prevent constipation:
- Make sure you drink enough liquids (six to eight cups per day).
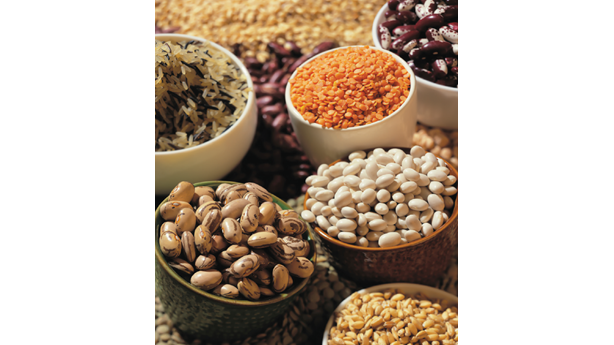
- Increase the amount of fibre in your diet. Whole grains and legumes such as lentils and kidney beans are good sources of fibre.
- If water and dietary fibre do not help prevent constipation, speak to your healthcare provider about over-the-counter products that may be helpful.
- Keep as active as you can.
Retraining
Your healthcare team may suggest retraining. This involves going to the toilet on a regular schedule, for example every two hours for bladder, every morning for bowel.
Refusing liquids is not a good strategy
No matter the cause of your problems, it is very important to drink enough liquids to prevent dehydration — six to eight cups per day.
Where to get support
Physiotherapists can teach you pelvic floor exercises that strengthen the muscles you need for control.
Occupational therapists can help make it easier to get to and use the toilet.
Nurses can help with skin care and tips for retraining.
Dietitians can help you choose high-fibre foods and plan ways to drink more liquids.
